The Hidden Risks of Over-Sanitization: How Excessive Hygiene Affects Immunity and Allergies

In today’s world, cleanliness is often equated with health. From antibacterial soaps to hand sanitizers, disinfectants, and rigorous cleaning routines, we have been taught that staying germ-free is the key to preventing illness. While maintaining hygiene is undeniably important—especially in preventing infectious diseases—there is a growing body of research suggesting that excessive sanitization may come with unintended consequences for our immune system. This phenomenon, often referred to as the "hygiene hypothesis," proposes that over-sanitization and reduced exposure to microbes in early life can increase susceptibility to allergies, autoimmune diseases, and other immune-related disorders.
Understanding the Hygiene Hypothesis
The hygiene hypothesis was first proposed in the late 1980s by epidemiologist David Strachan, who observed that children growing up in larger families, exposed to more infections, had lower rates of hay fever and allergies. Since then, many studies have expanded on this idea, linking a decrease in early microbial exposure to a rise in immune disorders.
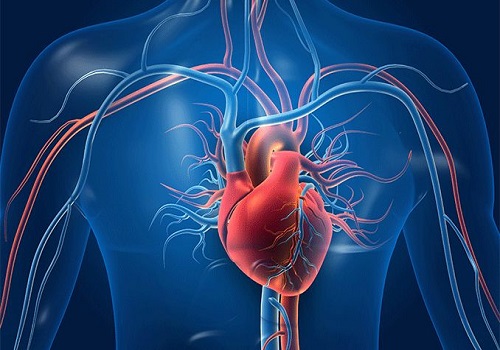
The immune system requires a certain level of “training” to learn to distinguish between harmful pathogens and harmless substances. This training largely happens through exposure to a diverse array of microorganisms—bacteria, viruses, and fungi—especially in childhood. When we excessively sanitize our environment, we limit these exposures, which may impair immune regulation and increase the risk of allergic and autoimmune responses.
How Over-Sanitization Impacts Immunity
Reduced Microbial Diversity: Regular use of strong disinfectants and antibacterial products not only kills harmful pathogens but also beneficial microbes that help balance our microbiome—the community of microorganisms living in and on our bodies. A diverse microbiome is essential for proper immune function.
Immune System Imbalance: Without adequate microbial exposure, the immune system may become hyperreactive, mistaking benign substances like pollen, pet dander, or certain foods as threats, triggering allergic reactions.
Increased Allergies and Asthma: Research has linked environments that are too clean to higher rates of asthma, eczema, and food allergies. For instance, children raised in overly sterile settings show higher incidences of these conditions compared to those who grow up on farms or in environments with rich microbial exposure.
Autoimmune Disorders: Some autoimmune diseases, where the immune system attacks the body’s own tissues, are thought to be influenced by lack of microbial exposure. The immune system fails to learn tolerance without sufficient microbial "education."
Striking the Right Balance: Hygiene Without Overdoing It
While the dangers of over-sanitization exist, it’s important to clarify that good hygiene practices—such as regular hand washing, safe food preparation, and cleanliness in healthcare settings—remain critical in preventing infections and diseases. The goal is to find a balance that protects us from harmful pathogens without depriving our immune systems of necessary microbial interactions.
Practical Tips for Balanced Hygiene
Use Soap and Water Over Antibacterial Products: For routine hand washing, plain soap and water are usually sufficient and do not disrupt beneficial microbes as aggressively as antibacterial soaps.
Avoid Excessive Use of Disinfectants at Home: Reserve disinfectant sprays and wipes for high-risk areas (like kitchens and bathrooms) rather than sterilizing every surface multiple times daily.
Encourage Outdoor Play for Children: Exposure to natural environments helps build a diverse microbiome and strengthens immune resilience.
Limit Unnecessary Antibiotic Use: Antibiotics kill both harmful and beneficial bacteria; avoid their use unless medically necessary.
Eat a Microbiome-Friendly Diet: Include fermented foods, fruits, vegetables, and fiber-rich foods that nourish gut bacteria.
Future Research and Innovations
The scientific community continues to explore the complex relationship between hygiene, microbiome diversity, and immune health. Emerging therapies, such as microbiome transplantation and probiotics tailored to immune modulation, offer promising avenues to restore balance where needed.
Moreover, public health messaging is evolving to emphasize "targeted hygiene"—focusing on hygiene practices that reduce disease transmission while preserving beneficial microbial exposure.
Conclusion
The COVID-19 pandemic has understandably heightened awareness about hygiene, leading to widespread use of sanitizers and disinfectants. However, it’s crucial to remember that our immune system thrives on a certain level of microbial exposure. Over-sanitization may inadvertently contribute to the rising prevalence of allergies and autoimmune diseases by disrupting immune system training and microbiome balance.
By adopting balanced hygiene practices, encouraging natural microbial interactions, and maintaining a healthy lifestyle, we can protect ourselves from infectious diseases while supporting long-term immune health.