mRNA-based stem cell therapy offers hope for chronic & acute liver disease
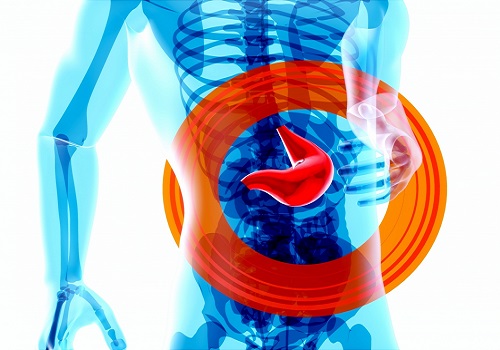
A novel stem cell treatment, using mRNA technology encapsulated into nanoparticles (LNP) that was successfully used to produce the Covid-19 vaccines, may help in the treatment against chronic and acute liver disease.
Liver transplantation remains the only treatment for end stage liver disease, but there is a critical shortage of organ donors, necessitating a dire need for new forms of treatment.
The research from Boston Medical Center and Boston University showed that the mRNA based stem cell therapy can boost the natural repair mechanism of the liver to regress the diseased tissue caused by either an acute or chronic liver injury.
Published in the journal Cell Stem Cell, researchers identified a specific receptor present on the stem cells which can be recognised and activated by the ligand protein called vascular endothelial growth factor A (VEGFA).
“This potential treatment has important clinical implications for people suffering from chronic liver disease, allowing the liver to heal itself, and potentially avoiding the need for many liver transplants,” said corresponding author Valerie Gouon-Evans, Director of the Boston University Liver Biologist Programme.
“It’s our hope that these findings, with further study, will be translated to clinical patient care to alleviate chronic liver disease and the need for transplants as a result of acute or chronic injury,” Gouon-Evans added.
The liver is known for its remarkable regenerative ability through proliferation of hepatocytes. But during chronic injury or severe hepatocyte death, proliferation of hepatocytes is exhausted.
To overcome this hurdle, researchers studied VEGFA as a therapeutic means to accelerate biliary epithelial cell (BEC)-to-hepatocyte conversion.
Researchers used mice and zebrafish liver disease models. In the zebrafish studies, the liver disease was created by inducing hepatocyte death with genetic and chemical intervention. The experimental group of fish was then exposed to overexpression of VEGFA while the control group was not.
They observed a significant increase of newly generated hepatocytes from the BEC-derived stem cells in the presence of VEGFA.
In the mouse study, the acute disease was induced with an overdose of the drug acetaminophen, and the chronic disease was promoted with a diet. The experimental groups were treated with 2 injections of VEGFA mRNA-LNP, while the control groups were injected with neutral mRNA-LNP.
Researchers demonstrated that delivery of VEGFA mRNA-LNP in both acutely or chronically injured livers induced robust BEC-to-hepatocyte conversion with a five-fold increase compared to control-treated mice, and importantly full reversion of steatosis and fibrosis in the chronic model.
This treatment activates the stem cells of the liver, a subset of the biliary epithelial cells (BEC) lining up the liver biliary tree, so that they proliferate and generate new healthy hepatocytes, the functional cells of the liver